Loma Linda University Health is using the latest technology to improve quality of life.
Echocardiography is a non-invasive imaging modality that has revolutionized the field of cardiology with its ability to provide detailed, real-time images of the heart’s structure and function. In the intricate world of cardiac care, echocardiography (ECHO) often marks the crucial first step in a patient’s journey toward diagnosis, treatment, and improved heart health, says Ramesh Bansal, a professor at the Loma Linda University School of Medicine and former medical director of the ECHO lab at Loma Linda University International Heart Institute.
For decades, the International Heart Institute’s ECHO lab has aided in early detection and diagnosis and played a pivotal role in guiding treatment decisions and monitoring cardiac conditions.
“When our expert team at International Heart Institute performs an ECHO in patients with complex structural heart conditions, it leads to early diagnosis, surgical planning, and better outcomes,” Bansal says.
For patient Steve Bloch, a 63-year-old former firefighter and helicopter pilot, a life-threatening cardiac event led him to understand the significance of cardiac imaging using ECHO. Bansal first diagnosed Bloch with an abnormal heart valve in 1992; an ECHO revealed Bloch was born with two instead of three leaflets in his aortic heart valve. If left unmonitored and untreated, Bloch’s condition, known as bicuspid aortic valve, could cause his aorta, the body’s largest artery, to dilate (aortic aneurysm) or tear (aortic dissection).
Bansal advised Bloch to seek ECHO checkups every year to prevent this fate. But it wasn’t until a decade later, in 2003, that Bloch returned to LLUH to be treated for his dangerous aortic dissection. Bloch went to the operating room, where Bansal used an advanced imaging technique called transesophageal echocardiogram (TEE) to supply the cardiac surgeon with vital information about the tear in his aortic valve. Research from LLUH has demonstrated the advantages of TEE in treating patients with aortic dissection.
Aortic dissection is a potentially lethal cardiac disorder with an average surgical mortality of 25 percent, according to data from the International Registry of Aortic Dissection (IRAD). A study of more than 150 patients conducted at LLUH reported the mortality was less than 10 percent for such patients treated at LLUH. He says the International Heart Institute’s multi-disciplinary expertise and state-of-the-art technology enable care teams to guide patients with aortic disorders through diagnosis, treatment, and healing.
Bloch has followed up with Bansal for regular ECHOs since 2003, grateful to experience milestone moments such as celebrating 38 years of marriage with his wife, witnessing his daughter graduate, and watching his granddaughters grow.
“ECHOs are unassuming because they are pretty quick and painless, but they give such valuable information that could make experiences like mine preventable,” Bloch says.
Bansal says he and other International Heart Institute experts are equipped to recognize and treat even the rarest, most complex of conditions, including congenital heart disease (CHD). Only 1 percent of live births in the U.S. are found to have CHD — a heart defect at birth — Bansal says. With advances in medicine, he says more children with CHD have lived to adulthood — currently more than one million adults — and require specialized, lifelong care and treatment for their conditions. Bansal says under his guidance over the years, the ECHO lab team has become a leader in the region in caring for the growing population of adults with CHD.
Leslie Forte has lived with a type of CHD known as tetralogy of the fallot (TOF) for 35 years. She had her first heart surgery as a baby and started her care with Bansal in 2019. He performed an ECHO and discovered a leaky pulmonary valve and a hole called patent foramen ovale (PFO) in her heart that wasn’t previously known. She opted for open-heart surgery to fix her heart in 2022, during which Bansal provided TEE guidance for surgeon Anees Razzouk, to optimize outcomes.
Cardiac imaging experts play a crucial role during complex cardiac interventions (such as transcatheter edge-to-edge mitral valve repair) and surgeries by providing real-time imaging guidance to the medical team, Bansal says.
“This is the only center in the region that can provide care services from A to Z for every heart patient, no matter how intricate their case may be,” he says.
Aside from helping to treat heart valve disorders and CHD, ECHO also proves essential to diagnosing and monitoring other heart conditions. Brian Kelley has undergone regular ECHOs since 2008, shortly after his diagnosis of hypertrophic obstructive cardiomyopathy (HOCM) — a rare disease, in most cases inherited, where the heart’s left ventricle muscle is thicker than average and can hinder the exit of blood flow from the heart.
The condition places people at risk of sudden death, Bansal says. He uses ECHO as an essential tool for risk assessment, analyzing the heart’s high-risk features, such as muscle thickness, how well the heart pumps blood (ejection fraction), and the presence of an apical cardiac aneurysm. Bansal deemed Kelley at risk of sudden death and recommended he receive an Implantable Cardioverter-Defibrillator to save the heart from life-threatening abnormal heart rhythms.
Years later, Kelley’s ECHOs showed that his thickened heart walls were blocking his blood flow, so he underwent a double myectomy to relieve two levels of obstruction in his heart. Once again, Bansal provided TEE guidance during the procedure to support surgeon Razzouk in safely removing Kelley’s obstructions.
Genetic testing had revealed Kelley possessed a gene mutation for the condition that could be passed on, so he and his wife worked with Bansal to test their children for the same condition when they were born. Both of their children inherited the condition, for which they now receive frequent ECHOs to safeguard their health.
“We are grateful to Dr. Bansal and the cardiology team who have provided our family with the absolute best care over the years,” says Kelley’s wife, Jenni, a pediatric cardiac ICU nurse. “They are professional, efficient, and use the most recent advancements in cardiology to care for our family.”
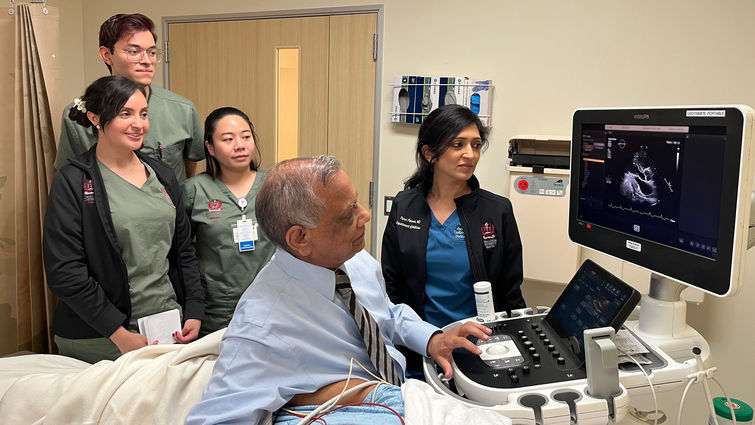
An entourage of students have studied Kelley’s condition as part of their training, says Bansal, who started the Ultrasound/Sonography program at Loma Linda University School of Allied Health Professions. Bansal has supervised the ECHO lab’s growth as its director since 1983 and handed off his role earlier this year to cardiac imaging expert Purvi Parwani, while he continues to serve patients and the ECHO lab.
“We are so proud to provide our expertise and cutting-edge imaging services to help patients handle any kind of problem in the heart, whether simple or highly complex,” he says. “Although there are multiple other modalities available for heart patients at LLUH, such as CT or MRI, it all starts with ECHO, where our utmost duty is to do the best for patients’ well-being.”
The original version of this story was posted on the Loma Linda University Health news site.















