Loma Linda’s Andrew Woodward shares tips to follow during oncological treatment.
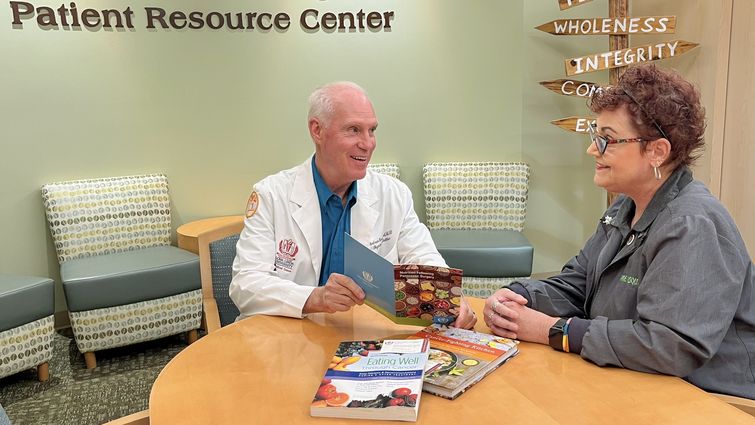
Many people with cancer grapple not only with their disease and treatment but also added hurdles of ensuring they eat enough and properly throughout treatment. Maintaining appetite and consuming enough nutrients can prove difficult for patients with cancer, says Andrew Woodward, an oncology nutritionist at Loma Linda University Cancer Center, yet they can develop various strategies to safeguard dietary health and overall well-being.
Cancer treatment and cancer itself can cause changes in appetite, Woodward says, with each person’s disease and reaction to treatment differing. He says some patients may eat less than usual, feel full quickly, or not feel like eating. Others may experience nausea, vomiting, mouth sores, or changes in food’s taste or smell that lower appetite. Last but not least, he adds that patients’ psychological and emotional states also strongly influence appetite and eating habits.
Loss of appetite can lead to patients’ undernutrition or malnutrition — called cachexia in the context of chronic illnesses, including cancer. Cachexia and nutrient deficiencies can lead to debilitating health consequences, Woodward says, including muscle wasting, weakness, depression, dehydration, and hindrance of brain functions such as memory and information processing.
Patients can ensure they eat enough and eat well by partnering with nutritionists like Woodward, with whom they may discuss their circumstances and develop personalized strategies to mitigate appetite loss. Woodward says assuming a one-size-fits-all solution to cancer-related appetite loss is ineffective in addressing each patient’s unique challenges and concerns. Instead, Woodward investigates each patient’s personality, culture, and food preferences to tailor eating recommendations.
“When patients tell me food tastes bad, I ask them to explain in more detail so that I can determine best-suited recommendations,” he says. “Does food lack flavor, taste bitter, or taste like it has metal shavings in it? If the patient says food is tasteless, I recommend herbs and condiments that can boost flavors, whereas if their food tastes metallic, citrus or even pickles can help cleanse the palette. One of my patients bites into a pickle before eating a meal to get rid of that bad taste.”
Woodward accounts for three interwoven factors in the management of patients’ appetites:
Physiology. The type and location of cancers can affect appetite differently. For instance, Woodward says cancers in the gastrointestinal tract may directly affect satiety or the feeling of fullness. The cancer’s location can also trigger other effects that lower appetite, like nausea. Large-sized tumors can produce pro-inflammatory cytokines, substances that influence the brain and nervous system to reduce appetite.
Psychology. Woodward says a patient’s mental and emotional state, way of coping with cancer, and their support system can significantly influence eating habits and appetite. For instance, he has observed that patients with loving significant others who can help with food prep and encourage eating tend to have better outcomes than patients without such support systems. He adds that food is often enjoyable and meaningful because it symbolizes love.
Patients dealing with mental health illnesses such as depression may eat less. Woodward recommends fostering an environment that is as calming and pleasant as possible in preparation for a meal, as opposed to a tense and stressful atmosphere. He encourages patients to pursue whole-person care by relying on support systems and seeking help from mental health professionals and oncology nutritionists.
Pharmacy. Woodward says at least five different medications can be useful to stimulate appetite for patients with cancer who struggle to eat. Some of these medications also provide benefits to control nausea or help with mood. As an oncology nutritionist, Woodward says he identifies situations where patients would benefit from medications and coordinates with patients’ oncologists to determine the best course of action regarding medication type and dosage.
“It’s a tug of war where the patient knows they need to eat, but they just don’t have the desire to eat,” Woodward says. “Partnering with a nutritionist can really help patients make sure they’re getting enough to eat and improve the quality of nutrition they need in a way that works for them.”
Some Recommendations
Woodward shares some of the recommendations he offers patients facing appetite loss — each of which can be modified to fit specific needs and preferences.
Small, frequent meals. Patients with low appetite who may experience other side effects from treatment might be unable to eat normal portions at once. In these cases, Woodward encourages eating small meals and snacks every two or three hours in the day.
Protein drinks. Protein drinks are valuable when consumed in addition to regular meals, Woodward says. With more than different kinds to choose from, he says, he works with patients to personalize their options and offers various flavoring ideas to improve the drink’s taste for patients. He says protein drinks are portable, convenient, adaptable, and effectively add necessary proteins and calories to a diet and help patients maintain a stable weight. It’s crucial that patients don’t replace meals with protein drinks but consume them between meals to “receive more nutrition per swallow,” Woodward says.
Positive affirmations. Woodward encourages patients to engage in positive self-talk as they prepare a meal or eat their food. Some of his examples include: “I honor my body with healthy food,” “I want to fuel my body,” or “I want to rebuild my body.” He says positive affirmations can help patients claim ownership of their food and body and serve as helpful reminders of the food’s role in their well-being.The original version of this story was posted on the Loma Linda University Health news site.