Pancreatic cancer survivor calls other patients to never give up.

Pancreatic cancer is associated with poor outcomes — according to the U.S. National Cancer Institute, only 12 percent of people diagnosed with pancreatic cancer are alive five years after their diagnosis. Physicians and researchers within the medical community at Loma Linda University Cancer Center are actively working to improve the effectiveness of pancreatic cancer care by combining their expertise, personalized patient care, and clinical trials investigating new treatment approaches.
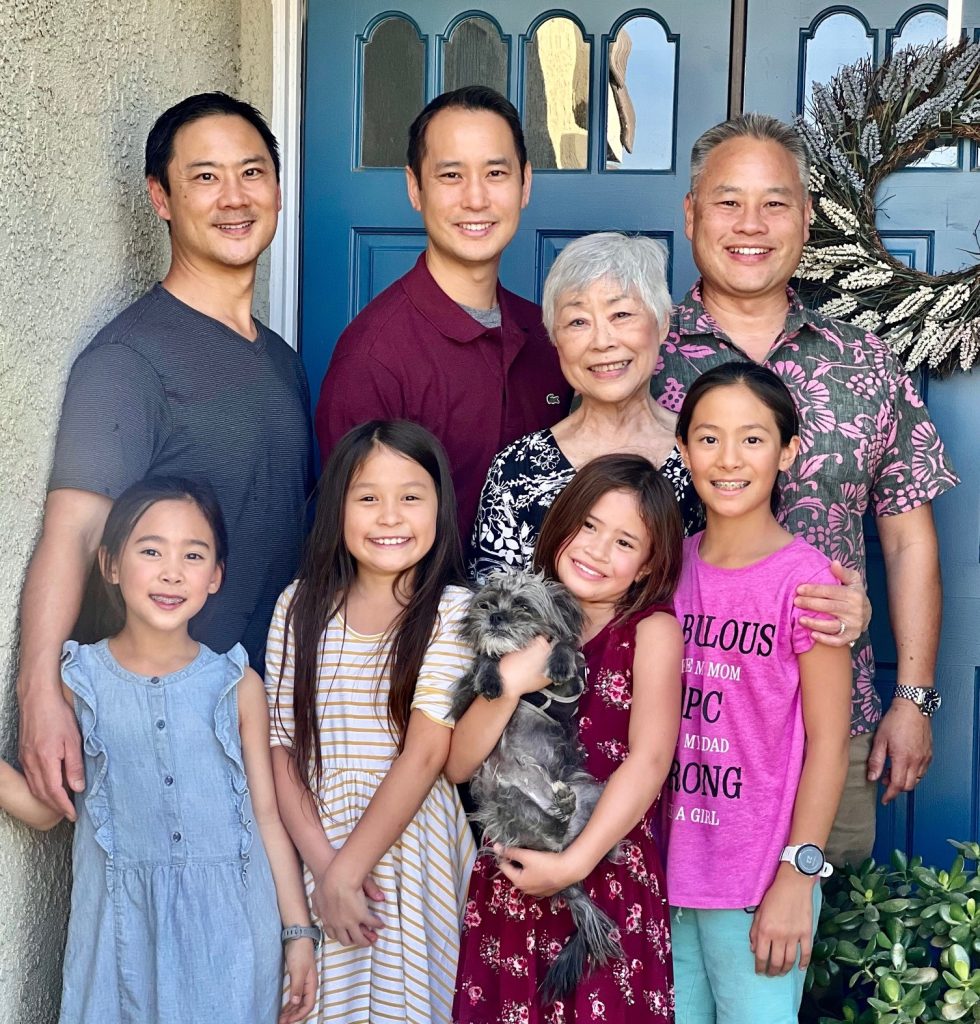
These factors, combined with patients’ tenacity and robust support systems, enable some to survive and thrive years after diagnosis, such as 77-year-old Jean Hwang, who celebrates two years with no evidence of cancer.
Pancreatic cancer symptoms usually become apparent only after the cancer has grown very advanced, Michael P. O’Leary, a surgical oncologist at Loma Linda University Cancer Center, said. As a result, pancreatic cancer is often diagnosed after it has already spread, making it difficult to treat. Yet 1 in 5 diagnosed patients have a tumor that hasn’t spread and is still resectable. When cancer is deemed resectable, physicians can remove the mass through a highly complex surgery called a Whipple procedure that can potentially cure patients.
Such was the case for Hwang, who told her doctor in 2020 about her symptoms of fatigue, dark urine, and light-colored stool. Bloodwork and scans identified a tumor that had formed at the top of her pancreas and was blocking her bile duct (thus causing her symptoms). Hwang’s four children, all Loma Linda University alums, insisted she receive care at Loma Linda University Cancer Center.
After evaluating her scans, the Cancer Center team deemed the cancer resectable, says O’Leary. Experts determine whether patients are eligible to have their pancreatic cancer removed if the tumor does not interfere with other major blood vessels in the region.
However, studies have found that when eligible patients undergo the physically taxing Whipple procedure, they are less likely to be able to receive chemotherapy afterward. The Cancer Center had launched a clinical trial to investigate a new option: whether receiving chemotherapy before the Whipple surgery could prove beneficial to patients.
“Considering the poor prognosis for pancreatic cancer, it is clear that we need to change how we’re treating cancer because those numbers are unacceptable,” O’Leary says. “We are constantly looking for novel approaches to therapy through research and clinical trials and investigating ways to improve survival.”
When Hwang learned about the clinical trial from Mark Reeves, surgical oncologist and director of the Cancer Center, she decided to enroll.
“I agreed to participate in the trial because I just trusted my surgeon Reeves and the care team with my life,” she says. “It sounded like a good plan.”
But her treatment was delayed when she and her husband contracted COVID. In a matter of days, she lost her husband of 51 years and was hospitalized in January 2021 — a “horrendous” start to her year. Yet Hwang began her chemotherapy as soon as she recovered from COVID. She developed a liver abscess amid treatment that landed her back in the hospital for nearly another month; care teams and her children eventually nursed her back to health.
“I was so weak that I had to relearn to walk and feed myself, but I gradually got stronger and never gave up,” she says.
Hwang says she joined online support groups for pancreatic cancer and Whipple survivors during this difficult time. Reading others’ stories helped lift her spirits and encouraged her to keep going. Now, she hopes sharing her story can help others in need.
“Maybe God allowed me to live so I can encourage people,” she says.
By spring 2021, Hwang completed chemotherapy and began proton therapy, a targeted way of delivering radiation directly to an area affected by the tumor. Finally, she underwent the Whipple procedure in the summer of 2021. She says she felt confident that she was in good hands and appreciated when staff members offered to pray with her before her surgery.
“The morning of my surgery, I was really calm and felt at peace when I went in,” she says.
Her 10-hour surgery entailed removing a portion of the pancreas, stomach, the first part of the small intestine (duodenum), the gallbladder, and a portion of the bile duct. After six weeks of recovery and taking oral chemotherapy, all her scans have returned clear.
Over the past two years, Hwang has enjoyed spending time with her children and eight grandchildren. As a musician and former symphony member, Hwang delights in teaching piano to her granddaughters and her neighbor’s grandson. She has traveled to Hawaii and cruised across parts of Europe. For November’s Pancreatic Cancer Awareness Month, she will share her story at a local church and play music with her son.
“I have so much to be thankful for,” she says. “I just want to encourage people not to give up.”
O’Leary says that although pancreatic cancer is a challenging diagnosis, he holds a lot of hope for those patients.
“Pancreatic cancer is often a devastating diagnosis,” he says. “It is a privilege to partner with patients to help them deal with the diagnosis, manage and relieve their symptoms, and sometimes, achieve a cure.”
The original version of this story was posted on the Loma Linda University Health news site.








