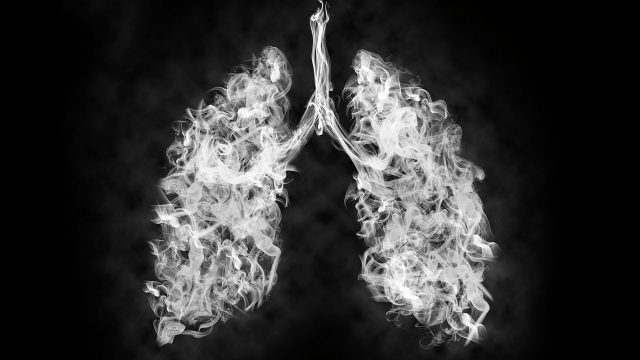
Adventist HealthCare is ramping up its services to assist patients with kidney failure.

To better accommodate rehabilitation inpatients in need of dialysis, Adventist HealthCare Rehabilitation, based in Maryland, United States, offers in-house hemodialysis services close to home.
“We felt it important for patients to receive hemodialysis on-site instead of being transported to another facility,” Rob Grange, vice president and Post-Acute Care Services administrator at Adventist HealthCare Rehabilitation White Oak, said. “From quality and convenience standpoints, this is a big win, as on-site hemodialysis reduces cost and risk for patients.”
The U.S. Centers for Disease Control and Prevention estimates that 37 million people in the country live with chronic kidney disease. For optimal results, patients must receive kidney care multiple times per week, which can cost patients a significant amount of time and money associated with travel and can be stressful for patients receiving rehabilitation as an inpatient. On-site hemodialysis addresses that problem and aids in recovery.
On-Site Hemodialysis Builds Patient Trust
Adventist HealthCare Rehabilitation began offering on-site hemodialysis in 2020. Before then, rehabilitation inpatients in need of the service faced a dilemma. They either required daily transport to another facility for dialysis care or had to recover in a skilled nursing or rehabilitation facility farther from home.
Patients who chose daily transport experienced substantial obstacles to optimal care, such as fatigue, which reduced their likelihood of undergoing therapy at the proper intensity. Those who transferred to other facilities had less access to the support of family and friends.
In most cases, hemodialysis takes approximately four hours. Depending on what part of the day dialysis is conducted, the patient spends the other portion of the day receiving expert care from therapists and the nursing staff. Bringing these hemodialysis services in-house, the Adventist HealthCare Rehabilitation team not only adds convenience for patients but also improves coordination of care between rehabilitation specialists and administrators of hemodialysis, as they all work within the same building and have immediate access to one another.
Until 2019, Adventist HealthCare Rehabilitation served approximately 15 inpatients a year who required dialysis services along with their rehabilitation. Since bringing in-house hemodialysis to Adventist HealthCare Rehabilitation Rockville in 2020 and Adventist HealthCare White Oak Medical Center in 2021, the number has grown exponentially. During 2021, rehabilitation staff served 43 such inpatients — a growth of nearly 200 percent. The program is on track to help a similar number of patients in 2022.
The need for frequent hemodialysis care is not unique to the surrounding Prince George’s and Montgomery counties. From 1980 to 2017, the United States Renal Data System (USRDS) found that the number of Americans with end-stage renal disease increased dramatically. The USRDS report found hemodialysis to be the predominant form of first-line therapy among those with end-stage renal disease, illustrating a growing need for such services in outpatient and inpatient settings.
“Adventist HealthCare Rehabilitation’s inpatient hemodialysis program has room to grow,” Grange said. “The program leaders will likely embrace the extra capacity in the coming years to meet the growing number of residents who will receive hemodialysis.”
Monitoring Results to Improve Future Services
Many patients needing inpatient rehabilitation services get referred to Adventist HealthCare Rehabilitation following a stroke, bone fracture, or other life-altering event. They come from nearby acute care hospitals in the area and even Washington, D.C. Whatever their rehabilitation requirements or distance from home, bringing hemodialysis in-house improves the patient experience and reduces one potential barrier to care.
“We really care about meeting our vision, which calls us to provide a world-class experience to every person, every time,” Grange said. “We’re passionate about identifying the things that keep us from meeting our vision.”
Hemodialysis, he explains, was the main identified obstacle leading patients to seek care elsewhere. This insight came from constant monitoring, a cornerstone of Adventist HealthCare Rehabilitation’s operating procedures. Having addressed the issue of hemodialysis, Adventist HealthCare Rehabilitation continues reviewing data to determine other services that would best serve inpatient rehabilitation patients. Adventist HealthCare Rehabilitation is giving more attention to a growing need for access to behavioral health services.
“Patients don’t come to us for psychiatric care, but such issues are often comorbidities within the rehabilitation patient population,” Grange said. “We want to make sure we have support in place to care for the mental and physical well-being of those undergoing inpatient rehabilitation.”
Grange anticipates adding behavioral health services to inpatient rehabilitation as early as 2023. Additionally, Adventist HealthCare Rehabilitation is prioritizing changes at the Rockville and White Oak facilities to better serve patients who require special accommodations due to obesity.
“We don’t want weight to be a reason not to attend rehabilitation,” Grange said.
Current equipment permits the admission of patients up to 400 pounds (180 kilograms). Adventist HealthCare Rehabilitation is developing processes that will allow the entry of qualifying patients weighing up to 750 pounds (340 kilograms).
“On-site hemodialysis, psychiatric care, and the ability to care for bariatric patients are some of the many things that make our inpatient rehabilitation services stand out,” Grange said. “We strive to continually grow that list to benefit patients and better serve referring physicians.”
The original version of this story was posted by Adventist HealthCare.